⭐
Obstructive Sleep Apnea (OSA) Optimization Program
A physician-led diagnostic and treatment pathway for better sleep, sharper cognition, lower blood pressure, and longer life.
Why OSA Matters
OSA is not just snoring
It is:
A cardiovascular disease (hypertension, arrhythmias, coronary risk)
A metabolic disease
A neurologic disease
A major contributor to daytime fatigue and weight gain
Untreated sleep apnea increases:
Hypertension
Atrial fibrillation
Stroke
Heart failure
Insulin resistance
Depression
Motor vehicle accidents
Cognitive decline
Treating OSA often improves a patient’s entire life within weeks.
What Makes My Program Different
Most clinics prescribe CPAP but offer little guidance on how to use it correctly.
My program is:
Personalized
Thorough
Physician-supervised
Designed for comfort, adherence, and long-term success
You are not a “download and data point.”
You are a human being whose sleep determines your health.
1. Screening & Diagnostic Evaluation
STOP-BANG Assessment
We screen for:
Snoring
Tiredness
Observed apneas
Blood pressure elevation
BMI
Age
Neck circumference
Gender
A score ≥3 = high risk.
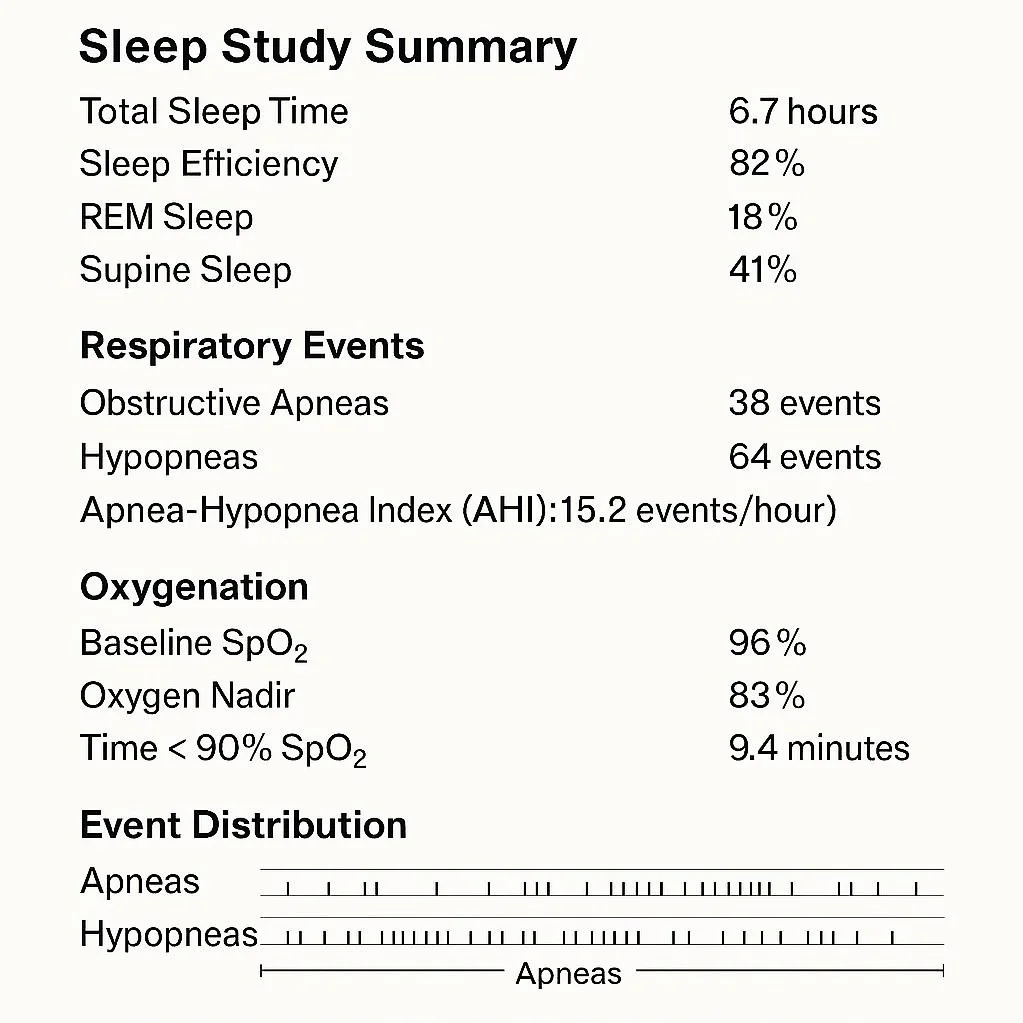
2. Home Sleep Testing (HST)
Most patients qualify for an at-home diagnostic test.
I coordinate:
Ordering
Delivery
Technical support
Interpretation of results
Insurance documentation
HST identifies:
AHI (apnea-hypopnea index)
Degree of oxygen desaturation
Sleep fragmentation
Positional apnea patterns
If the study is borderline or shows suspected central apnea, we escalate to in-lab polysomnography.
3. Understanding the Biology of OSA
OSA is caused by:
Collapsing upper airway structures during sleep
Reduced neuromuscular tone
Increased neck/visceral fat
Supine sleep
Alcohol/sedative use
Nasal obstruction
Anatomical predispositions
It worsens:
Blood pressure control
Blood sugar regulation
Hunger hormones (ghrelin)
Weight gain
Morning headaches
Cognition and alertness
Treating OSA helps weight loss — and weight loss helps OSA.
4. CPAP/BiPAP Therapy — Done Right
Patients fail CPAP because no one teaches them how to use it correctly.
My program includes:
Mask fitting (nasal, pillows, full face)
Humidity adjustment
Pressure optimization
Strategies for mouth breathing
Claustrophobia solutions
Ramp settings for comfort
Follow-up support sessions
Most people can tolerate CPAP with a physician who understands the equipment and how to personalize settings.
5. Alternatives for CPAP-Intolerant Patients
Not everyone tolerates CPAP.
I help patients find the right alternative when appropriate:
• Mandibular advancement devices
Great for mild–moderate OSA or CPAP refusal.
• Positional therapy
Devices that keep patients off their back.
• Weight loss -GLP-1 dramatically reduces AHI
OSA improves rapidly with GLP-1 therapy — a powerful synergy.
• Surgery referrals (selected cases)
UPPP
Inspire (hypoglossal nerve implant)
Nasal surgery
• Myofunctional therapy
Strengthens lower airway muscles.
6. Follow-Up & Optimization
Good OSA care requires iteration.
I monitor:
AHI trends
Mask leak
Residual events
Oxygen saturation
Daytime symptoms
Morning BP
Adherence metrics
We adjust:
Pressure settings
Masks
Humidification
Positional guidance
Lifestyle factors
You will not be lost in the system.
7. Lifestyle & Weight Interventions
OSA interacts with:
Weight
Alcohol
Nasal congestion
Sleep posture
Medications (especially sedatives and soporifics)
Late-night meals
I optimize all contributing factors, including:
GLP-1 therapy for metabolic OSA improvement
Anti-inflammatory diet guidance
Strengthening of upper airway musculature
Sleep hygiene and circadian alignment
OSA is a systemic disease — and requires a systemic solution.
8. What You Can Expect
With treatment, most patients experience:
Improved daytime energy
Better concentration
Lower blood pressure
Better glucose control
Better mood
Reduced nighttime anxiety
Fewer headaches
Better weight loss
Stronger cardiovascular outcomes
Many patients tell me their OSA treatment is “life-changing” within 2–6 weeks.
9. Pricing Structure
Members
Initial OSA Evaluation: Included
Home Sleep Test: Provided at near-wholesale cost
CPAP/BiPAP Setup & Education: Included
Follow-Up Evaluation: Included
Mask refitting & optimization: Included
GLP-1 for metabolic improvement: Add-on standard pricing
Non-Members
OSA Evaluation: $195
Home Sleep Test: $195–$275 depending on vendor
CPAP Setup, Mask Fit, Training: $95–$145 (one-time)
Follow-Up Visit: $75
Your Physician’s Message
Sleep is the foundation of health — the first domino that affects every system of the body.
Treating OSA restores:
Energy
Cognition
Weight control
Blood pressure
Mood
Longevity
I want your sleep back — and your life restored.